Can rectal cancer come back after successful treatment?
This is one of the most common and valid concerns patients have.
According to Dr. Sandeep Nayak, an internationally acclaimed surgical oncologist in India, rectal cancer is indeed a curable disease. Still, like many other cancers, there is always a possibility of recurrence. He explains that timely detection and structured follow-up are key to successful management.
Dr. Nayak, a pioneer in minimally invasive cancer treatment, including robotic and laparoscopic surgeries, emphasizes that many cases of rectal cancer recurrence can still be treated effectively when caught early.

What Is Rectal Cancer Recurrence?
Rectal cancer recurrence refers to the return of cancer after initial treatment, either in the rectum or nearby tissues, or in distant organs. This can happen months or even years after the primary therapy.
There are three main types of recurrence:
- Local recurrence: Cancer returns in the same area where it started.
- Regional recurrence: It appears in nearby lymph nodes.
- Distant recurrence (metastasis): The cancer spreads to distant organs, such as the liver or lungs.
Even though treatments like surgery, chemotherapy, and radiation can remove or destroy visible cancer cells, some microscopic cells may survive and grow later, leading to recurrence.
How Common Is Rectal Cancer Recurrence?
The rectal cancer recurrence rate varies depending on several factors, including stage at diagnosis, treatment type, and follow-up compliance. Generally, recurrence is most likely to occur within the first two to three years after treatment.
Studies show that about 20–30% of patients may experience recurrence. However, with advanced techniques such as robotic and laparoscopic surgery, the recurrence risk has decreased significantly.
Minimally invasive approaches allow more precise tumor removal, better visibility, and quicker recovery, all of which contribute to an improved rectal cancer prognosis.
Causes and Risk Factors for Rectal Cancer Recurrence
Several factors can influence the recurrence of rectal cancer, including:
- Stage of cancer: Advanced stages have a higher recurrence risk.
- Margins after surgery: Even a few cancer cells at the edge of the removed tissue can lead to recurrence.
- Lymph node involvement: The presence of cancer in lymph nodes indicates a greater chance of recurrence.
- Tumor biology: Aggressive cell types tend to recur faster.
- Lifestyle and health factors: Smoking, obesity, poor diet, and lack of physical activity can contribute.
Dr. Sandeep Nayak explains that “Recurrence doesn’t always mean the treatment has failed. Sometimes, it is simply the result of cancer cells lying dormant and becoming active again later.”
Signs and Symptoms of Recurrence

Recognizing the warning signs early is crucial. Some common symptoms suggesting a possible recurrence include:
- Unexplained weight loss after initial recovery
- Fatigue or weakness that doesn’t improve with rest
- Bleeding in stools or any new rectal bleeding
- Changes in bowel habits, such as constipation or diarrhea
- Abdominal pain or bloating
- Vomiting or signs of intestinal blockage
Any new or persistent symptom should never be ignored. Reporting these early allows doctors to perform necessary tests and confirm whether the issue is related to recurrence or another cause.
How Doctors Detect Recurrence
Doctors use a combination of clinical evaluation, blood tests, imaging, and endoscopic procedures to detect recurrence. The key is consistent post-surgery monitoring.
Some commonly used tests include:
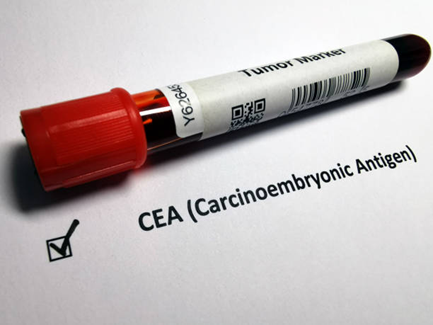
- CEA (Carcinoembryonic Antigen) blood test: A simple, inexpensive tumor marker test done every few months to track changes. A rising trend may indicate recurrence.
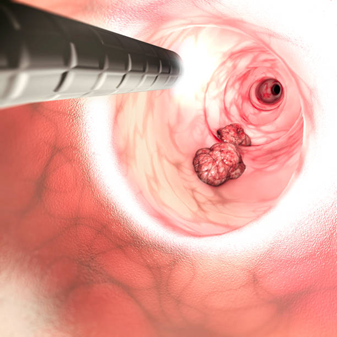
- Colonoscopy: Allows direct visualization of the rectum and colon to identify new growths or abnormalities.
- CT or PET-CT scans: Provide detailed images to detect any cancer cells that have recurred or spread.
Dr. Sandeep Nayak explains that these tests are performed at regular intervals in the first two years, then gradually less often to ensure recurrence is detected at the earliest possible stage.
Treatment Options for Recurrent Rectal Cancer
While recurrence can sound alarming, effective treatments are available. The approach depends on the site and extent of the recurrence.
Standard treatment options include:
- Surgery: For localized recurrences, minimally invasive or robotic surgery can remove the affected tissue with precision.
- Chemotherapy and radiation: Used to target cancer cells that cannot be surgically removed.
- Targeted and immunotherapy: Newer treatments that attack specific cancer pathways and boost the body’s defense mechanisms.
Preventing Rectal Cancer Recurrence

While not all cases are avoidable, following specific preventive strategies can lower the risk:
- Regular follow-up visits as advised by your oncologist
- A balanced diet rich in fiber, fruits, and vegetables
- Avoiding red and processed meat
- Maintaining a healthy body weight
- Engaging in regular physical activity
- Quitting smoking and limiting alcohol
Dr. Nayak emphasizes that recurrence prevention is not about controlling test results, such as CEA levels, but about monitoring overall health and early signs. As he explains, “Artificially lowering your CEA is like switching off the fire alarm; it doesn’t stop the fire.”
When to See Your Doctor
If you notice any of the following, contact your doctor immediately:
- Persistent bleeding
- Sudden unexplained fatigue
- Noticeable weight loss
- Change in appetite or digestion
- Any new lump or discomfort in the abdomen
Even if these symptoms turn out to be harmless, it’s better to be cautious. Timely evaluation ensures that any recurrence is detected while still treatable.
Conclusion
Frequently Asked Questions
1. What are the chances of rectal cancer coming back?
2. How soon does rectal cancer usually recur?
3. What are the signs that rectal cancer has returned?
4. How do doctors check if rectal cancer has come back?
5. Can lifestyle changes really reduce the risk of recurrence?
Reference
https://pmc.ncbi.nlm.nih.gov/articles/PMC4723445/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11640487/
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

