Low Anterior Resection Syndrome (LARS) is a common post-surgical condition observed in patients who undergo low anterior resection for rectal cancer treatment. It leads to bowel dysfunction, affecting the quality of life. LARS is a temporary problem that occurs as we save the anal sphincter and avoid permeant stoma.
According to Dr. Sandeep Nayak, a leading surgical oncologist in India, “LARS is a prevalent but manageable condition. With appropriate care, patients can regain bowel control and live comfortably. Timely symptom detection and effective management are crucial for this post-operative issue.”
With long-standing experience in surgical oncology, Dr. Nayak is an expert in complex colorectal cancer surgeries and post-surgery rehabilitation. With his team, he ensures patients receive individualized treatment protocols to deal with LARS effectively. Dr. Nayak and his team are well-known for their expertise in minimally invasive surgery and advanced cancer treatment in Bangalore, allowing quicker recovery with fewer complications.
What is Low Anterior Resection Syndrome (LARS)?
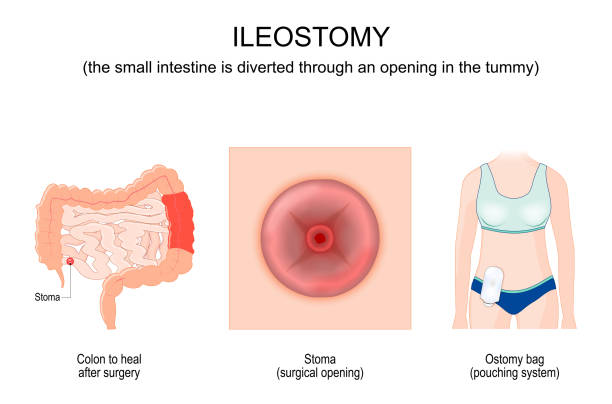
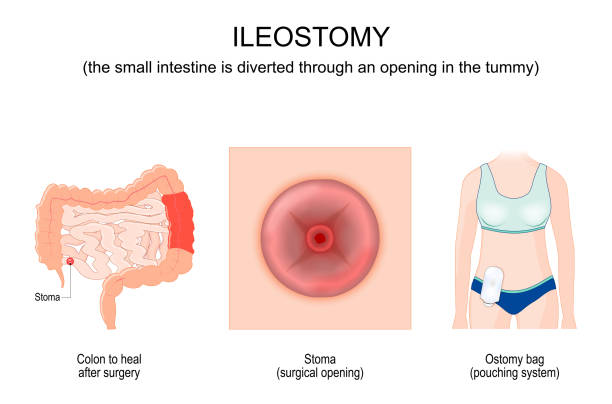
LARS is a group of symptoms occurring after low anterior resection (LAR). LAR is a surgical procedure designed to remove a portion of the affected rectum without removing the anal sphincter. LAR surgery is typically performed on patients with rectal cancer to maintain bowel continuity avoiding a permanent bag for stool collection, but can lead to bowel function abnormalities.
The rectum plays a vital role in controlling and storing stools.
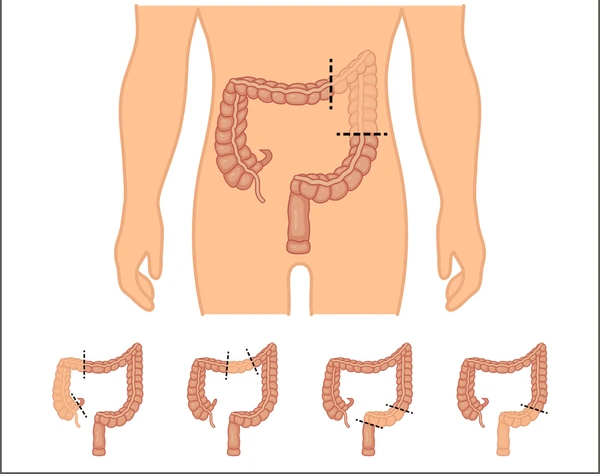
When a portion of the rectum is excised and modified, the body needs time to adapt, and the associated symptoms may persist for months to years. Adequate treatment and management of LARS can significantly improve the patient’s quality of life.
Do you have unexpected bowel changes after surgery? We will discuss the most frequent symptoms of LARS and how they impact daily living.
Symptoms of Low Anterior Resection Syndrome
Patients with LARS may experience:
- Frequent Bowel Movements– Needing to use the restroom multiple times daily.
- Fecal Incontinence– Some Loss of bowel control, with leakage at times, even when passing gas. This improves quickly after surgery.
- Bowel Urgency– Sudden, strong urge to defecate with little warning.
- Incomplete Evacuation– A sensation of not fully emptying the bowels.

- Constipation & Clustering – Alternating between hard stools and multiple small bowel movements in a short period.
- Gas and Bloating– Increased discomfort due to excess gas buildup.
- Unpredictable Bowel Habits– Irregular stool frequency and consistency, making daily life cumbersome.
- Nocturnal Bowel Movements– Bowel urges experienced at night, resulting in disturbed sleep.
“Most symptoms occur immediately after surgery. However, within one and a half to two years, most patients experience significant improvement and return to normal,” mentions Dr. Sandeep Nayak.
The severity of LARS symptoms is graded on a scoring system, which helps guide dietary modifications and other management strategies based on individual needs.
Identifying symptoms early can help control LARS better. Speak with a specialist for a personalized evaluation.
Managing Symptoms
The following strategies can help manage LARS:
- Dietary Adjustments
- Increase fiber intake gradually to regulate bowel movements.
- Avoid foods that trigger diarrhea, such as caffeine, dairy, and spicy foods.
- Stay hydrated to ease constipation and promote regularity.

- Pelvic Floor Exercises
- Pelvic muscle strengthening by some exercises can enhance bowel control.
- Kegel exercises tighten sphincter function and reduce incontinence.

- Toilet Routine
- Develop a regular bowel movement routine to promote regularity.
- Sit on the toilet and place a footstool to achieve an even better position for bowel emptying.
- Stress Management & Mental Well-being
- Reduce anxiety through meditation, breathing exercises, and counseling.
- Join support groups to connect with others experiencing similar challenges.

- Monitor Food Triggers
- Maintain a food diary to identify and exclude foods that trigger symptoms.
- Take small, frequent meals in order not to burden the digestive system.
Treatments for Low Anterior Resection Syndrome

Where lifestyle modifications are not sufficient, medical and sometimes surgical measures may be required:
- Medications– Loperamide anti-diarrheal medications delay bowel urgency, and fiber supplements thicken stools. Stool softeners may be used for constipation.
- Transanal Irrigation (TAI)– A method where the bowels are washed with water through a catheter to control the bowel movement and prevent incontinence.

- Dietary Counseling– A structured dietary plan created by specialists to balance fiber intake, avoid trigger foods and optimize digestion for better bowel control.
- Biofeedback Therapy– A technique that trains pelvic floor muscles to control bowel movement more effectively with the help of special sensors and therapist-guided exercises.
Conclusion
Low Anterior Resection Syndrome is a challenging condition, but with the right approach, symptoms can be managed effectively. From dietary changes to medical treatments, various ways exist to improve bowel function and enhance overall well-being. LARS will have to be managed in consultation with your treating doctors.
FAQs
What is anterior resection?
Anterior resection is a surgical procedure that removes a portion of the rectum affected by cancer while maintaining normal bowel function.
What is the best diet for low anterior resection syndrome?
A probiotic, fiber-rich, and well-hydrated diet can control bowel movements. Eliminate trigger foods such as milk, caffeine, and processed foods.
How long does low anterior resection syndrome last?
LARS symptoms last for years or months. Some patients recover slowly, but others need extended treatment.
What is the difference between anterior resection vs. low anterior resection?
Anterior resection involves the removal of upper segment of the rectum, whereas low anterior resection involves excising a lower portion of rectum while preserving the anal sphincter.
Reference links:
https://colorectalsurgery.wustl.edu/patient-care/low-anterior-resection-syndrome/
Disclaimer: This page is for informational purposes and not for promotional use.