Receiving a diagnosis of ovarian cancer after menopause can be overwhelming. As women age, the risk of ovarian cancer increases significantly. According to the American Cancer Society, around 75% of ovarian cancer diagnoses occur in women over the age of 55. Therefore, it’s crucial to understand this condition and seek expert guidance for effective management.
In this blog, we delve into the intricacies of ovarian cancer after menopause, shedding light on its symptoms, diagnosis and available treatment options.
Overview of Ovarian Cancer and its Prevalence in Post-menopausal Women
Ovarian cancer is a serious concern, particularly for women after menopause. It is one of the most common gynecological cancers. Unfortunately, the risk increases with age, especially for post-menopausal women.
This condition occurs when abnormal cells in the ovaries grow uncontrollably, forming tumors. While the exact cause is still unclear, factors such as age, family history, and genetic mutations play a role. Ovarian cancer usually goes unnoticed in its early stages because the symptoms can be subtle. Most of the ovarian cancers are detected in stage 3. Therefore, awareness are crucial for early detection and better outcomes.
Symptoms and Early Detection
Symptoms of ovarian cancer after menopause may include:
- Persistent abdominal bloating or swelling.
- Vaginal bleeding.
- Pelvic or abdominal pain.
- Changes in appetite or feeling full quickly.
- Frequent urination or urgency.
- Unexplained weight loss or gain.
- Changes in bowel habits, such as constipation
Challenges in early detection:
- Symptoms of ovarian cancer after menopause often mimic other common conditions, making diagnosis difficult.
- Many women mistake symptoms for typical signs of ageing or menopause, delaying medical attention.
- Ovarian cancer doesn’t have a reliable screening test like mammograms for breast cancer.
- The ovaries are deep within the body, making tumors more challenging to detect in routine exams.
- By the time symptoms appear, the cancer may have already advanced, making treatment more difficult.
“Stay vigilant and consult a specialist if you experience any of these symptoms, especially if they persist or worsen,” advises Dr. Sandeep Nayak, a highly regarded surgical oncologist in India. “Early detection is key to successful treatment.”
Don’t ignore any unusual symptoms. Schedule a check-up with a well-qualified professional today.
Understanding the risk factors for menopause ovarian cancer is key to prevention. Let’s explore how you can reduce your risk and stay healthy.
Risk Factors and Prevention
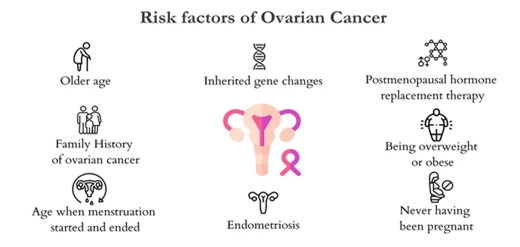
Factors that may increase the risk of ovarian cancer after menopause include:
- Age: Women over 55 have a higher risk.
- Family History: A family history of ovarian or breast cancer increases risk.
- Genetics: Inherited mutations in BRCA1 or BRCA2 genes.
- Hormone Replacement Therapy (HRT): Long-term HRT may slightly increase risk.
- Obesity: Being overweight or obese can elevate risk.
- Reproductive History: Never having children or having them later in life may increase risk.
- Endometriosis: Having endometriosis raises risk.
- Personal History: Previous breast, colorectal, or ovarian cancer diagnosis increases risk.
Prevention tips for ovarian cancer:
- Regular Check-ups: Routine ultrasound scan of abdomen can catch ovarian cancer early. (part of healthcheck)
- Healthy Lifestyle: Maintain a balanced diet and exercise regularly.
- Birth Control: Oral contraceptives can reduce the risk.
- Pregnancy and Breastfeeding: Having children and breastfeeding may lower risk.
- Genetic Testing: Consider genetic testing, especially if you have a family history of cancer.
- Surgical Options: Prophylactic surgery (removing ovaries and fallopian tubes) may be an option for high-risk individuals.
Though some factors can increase your risk of ovarian cancer, they don’t guarantee that you’ll develop it. Stay proactive with check-ups and a healthy lifestyle to reduce your risk as much as possible.
Learn about the diagnostic process and how staging is crucial in determining treatment options.
Diagnosis and Staging of Ovarian Cancer

- Diagnosis:
- Your journey begins with a series of diagnostic tests aimed at pinpointing the presence of ovarian cancer.
- Expect to undergo imaging tests, such as ultrasound or MRI or CT scans . These tests will help visualize any abnormalities in your ovaries or surrounding tissues.
- Blood tests, specifically the CA-125 test, may also be conducted. They help detect elevated protein levels associated with ovarian cancer.
- If the above tests are suspicious, your doctor may recommend a biopsy only if the disease is advanced. In suspected early cancers direct surgery is preferred as biopsy can rupture an early cancer and spread it. Biopsy involves taking a small sample of tissue and examining it under a microscope to confirm the presence of cancer cells.
- Staging:
- Once ovarian cancer is confirmed, staging becomes crucial in determining the extent of the disease and guiding treatment decisions. This is done using either a CT scan or PET CT scan.
- Ovarian cancer staging ranges from stage I (confined to one or both ovaries) to stage IV (spread to distant organs).
- Staging helps your medical team determine the most appropriate treatment approach, whether surgery, chemotherapy, or a combination.
- Furthermore, staging plays a vital role in predicting prognosis. Early-stage cancers typically have a better outlook than advanced-stage diseases.
H2 Treatment Options for Ovarian Cancer After Menopause
- Surgery:
Surgical removal of the cancerous tissue is often the primary treatment for menopausal ovarian cancer. The surgery is called Cyto-Reductive Surgery (CRS) and may be combine with Hyperthermia Intra-Peritoneal Chemotherapy (HIPEC) or Pressurized Intra-Peritoneal Aerosol Chemotherapy (PIPAC).
CRS surgery includes:
- Hysterectomy:
This is removal of uterus.
- Salpingo-Oophorectomy:
This surgery involves the removal of both ovaries and fallopian tubes.
- Lymph Node Dissection:
During surgery, nearby lymph nodes may also be removed to check for the presence of cancer cells. This helps stage the cancer and determine the best course of treatment.
- Omentectomy:
A fatty layer in the abdomen called omentum is removed.
- Peritoneum:
The involved peritoneum, the membrane lining the abdomen, may be removed if involved. This may be combined with removal of any other organ that is involved.

Depending on the extent of the disease and your health, your surgeon may opt for minimally invasive techniques, such as laparoscopic or robotic-assisted surgery. These approaches typically result in faster recovery and less postoperative discomfort.
- Chemotherapy:

This involves using potent drugs to destroy cancer cells. Chemotherapy may be given before or after surgery to shrink the tumor or kill remnant cancer cells.
- Targeted Therapy:
It includes drugs that target cancer cells while minimizing damage to healthy cells. These medications may be combined with chemotherapy or as a standalone treatment.
Your treatment plan will depend on various factors, such as:
- the stage and type of ovarian cancer
- your overall health
- your personal preferences.
It is essential to discuss all your options with your healthcare team. This will help determine the most suitable approach for you.
Consult a competent oncologist to explore personalized treatment plans suited to your needs.
Conclusion
If you’re experiencing symptoms like vague abdominal symptoms after menopause after menopause, don’t hesitate to reach out for help. Early detection is key in effectively managing ovarian cancer after menopause. Remember, knowledge is power, and by staying informed about the signs of ovarian cancer after menopause, you can take control of your health journey.
Dr. Sandeep Nayak, a prominent surgical oncologist in India, is here to guide you every step of the way. With his expertise and personalized care, you can confidently face menopause ovarian cancer.
Take the next step towards wellness today. Reach out for support and guidance.
Frequently Asked Questions:
1. Is it common to experience pain or discomfort in lower abdomen after menopause?
No. You should seek medical care if you experience any persistent pain or discomfort in the ovarian region or lower abdomen after menopause. This will help rule out any underlying issues.
2. What lifestyle changes can help prevent ovarian cancer after menopause?
The following lifestyle modifications can lower the risk of ovarian cancer after menopause:
- maintaining a healthy weight
- regular exercise
- quitting smoking
3. What are the survival rates for ovarian cancer after menopause?
Survival rates vary depending on factors like stage at diagnosis, overall health, and response to treatment.
4. What are the chances of recurrence of ovarian cancer after menopause?
The risk of recurrence depends on the stage and aggressiveness of cancer. CA125 levels are used as tumor marker for detecting recurrence. But, regular follow-up appointments are essential for monitoring.
5. Can I still lead a normal life after ovarian cancer treatment?
With proper treatment, support, and lifestyle adjustments, many women can lead fulfilling lives after ovarian cancer treatment. However, it may require some modifications and ongoing monitoring.