Can High Iron Levels Be a Sign of Cancer? |
High iron doesn’t mean cancer. Not automatically. Not even close to automatically. But persistently elevated iron that nobody has properly explained yet is a different conversation entirely. Because some cancers do change how the body handles iron in very specific ways. And the patients who act on that finding early are the ones whose options stay open longest.
According to Dr. Sandeep Nayak, surgical oncologist in India, “A persistently high ferritin without an obvious reason sitting in someone’s file for months without investigation is the kind of finding that keeps me up at night when I hear about it retrospectively.”
Which Cancers Actually Connect to Elevated Iron or Ferritin?
Not every high reading leads here. But specific patterns in specific people absolutely deserve more than a repeat test and a follow up appointment three months away.
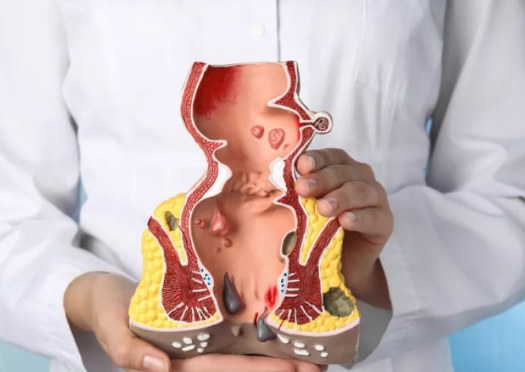
- Liver cancer: Hepatocellular carcinoma produces elevated ferritin both as a direct tumour marker and as a consequence of liver damage making persistently high ferritin in anyone with liver disease something that needs imaging now not later.
- Lymphoma: Hodgkin and non-Hodgkin lymphoma both drive ferritin dramatically higher through the inflammatory response they generate and markedly elevated ferritin sitting alongside unexplained fatigue and night sweats is a combination that nobody should be sitting on without investigation.
- Leukaemia: Acute and chronic leukaemias disrupt iron metabolism in ways that push serum iron and ferritin above normal range alongside the blood count changes that usually bring people into a clinic in the first place.
- Haemochromatosis related cancers: Genetic haemochromatosis causes iron to accumulate in organs over years raising lifetime liver cancer risk significantly and making iron overload not just a monitoring situation but an active and manageable cancer risk factor.
Elevated iron sitting alongside symptoms that don’t have another explanation is the combination worth taking seriously and catching it at the right moment is what makes liver cancer treatment genuinely curative rather than damage limiting.
What Else Causes High Iron That Needs to Be Ruled Out First?
Because cancer is not the first explanation and ruling everything else out properly is part of getting the answer right.
- Haemochromatosis: This inherited iron overload condition is one of the most common reasons adults have persistently elevated ferritin and most people carrying the gene have never once been screened for it despite it being straightforwardly testable.
- Chronic liver disease: Hepatitis B, hepatitis C, alcoholic liver disease and fatty liver all disrupt iron handling and push ferritin above normal in ways that reflect inflammation rather than malignancy but that still need investigation rather than an assumption that inflammation explains everything.
- Inflammatory conditions: Ferritin rises with any significant inflammation anywhere in the body including autoimmune disease, serious infection and chronic inflammatory conditions meaning a high ferritin can reflect something happening elsewhere entirely and still need proper investigation to confirm what it actually means.
- Repeated blood transfusions: Iron accumulates with multiple transfusions and produces elevated readings that only make sense when read alongside the patient’s full transfusion history rather than as a number sitting alone on a page without context.
If elevated iron has been sitting in your reports without a clear explanation it’s worth having a look at this to understand what proper investigation of liver related findings actually involves.
Why Choose Dr. Sandeep Nayak for Cancer Treatment in India?
Dr. Sandeep Nayak has spent more than 24 years treating liver cancers, lymphomas and complex malignancies where abnormal iron and ferritin readings were part of the diagnostic trail that led to the right answer at the right time. As one of India’s most experienced surgical oncologists he knows that a blood result is never just a number on a page. It’s a question sitting there waiting for someone to take it seriously enough to answer it properly. Every patient who comes to him with unexplained elevated markers gets a thorough clinical evaluation rather than another repeat test date and another deferral of the investigation that should have happened months ago.
Frequently Asked Questions
Does a high ferritin result always mean something serious is happening?
No, ferritin rises with inflammation, infection, liver disease and iron overload but any ferritin that stays persistently elevated without a clear identified cause needs proper investigation rather than ongoing monitoring that never actually looks.
What tests should be done alongside iron levels to get the full picture?
Full blood count, liver function tests, transferrin saturation, serum ferritin, CRP and LDH together tell a far more complete story than iron levels read in isolation from everything else going on.
Can cancer treatment itself push iron levels higher in patients already being treated?
Yes, repeated transfusions and certain chemotherapy regimens both disrupt iron metabolism in ways that need interpreting within the full clinical context rather than as standalone numbers disconnected from the treatment the patient is receiving.
When should persistently high ferritin prompt a specialist visit rather than just monitoring?
Any ferritin consistently above 500 micrograms per litre without a clearly identified benign cause deserves specialist evaluation rather than a monitoring plan that keeps deferring the conversation indefinitely.
Reference links:
-
American Cancer Society – Tests for Liver Cancer and Blood Markers
https://www.cancer.org/cancer/types/liver-cancer/detection-diagnosis-staging/how-diagnosed.html -
National Center for Biotechnology Information – Hyperferritinemia: Causes and Clinical Significance
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8125175/
- Disclaimer: The information shared in this content is for educational purposes and not for promotional use.