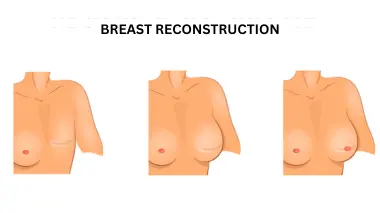
Breast cancer is not just a diagnosis; it’s a profound challenge that affects every aspect of a woman’s life, often leading to surgeries like mastectomy that can leave both visible and invisible scars. The loss of a breast can deeply impact a woman’s self-image and femininity, serving as a persistent reminder of her ordeal. Breast reconstruction can restore a woman’s confidence and help her feel whole again.
Dr. Sandeep Nayak, a surgical oncologist in India, explains:
“Breast reconstruction is a surgical process designed to restore the shape and appearance of a breast. This procedure can involve various techniques, ranging from implants to autologous tissue reconstruction, where the surgeon uses tissue from another part of the patient’s body to create a new breast. It’s a highly individualized surgery that can be performed immediately following mastectomy or delayed until a later date.
Has a mastectomy impacted your life? Please consult a qualified surgical oncologist or plastic surgeon to explore your options.
Are you curious about the process involved in rebuilding your breasts? Let’s break it down step-by-step.
Understanding Stages of Breast Reconstruction after Mastectomy
Consultation and Planning:
The first stage involves a detailed discussion with your surgeon to plan the breast reconstruction. The surgeon will explain different options and help you choose the best one based on your medical history and personal preferences.
Breast reconstruction can be performed at the time of mastectomy or at a later date which is called secondary reconstruction. The options of surgery differ based on various situations. This article covers only the secondary reconstruction.
Tissue Expansion or Implant Placement:
If opting for implants, the surgeon places a tissue expander under the chest muscle and gradually filled with saline over weeks or months. Once the skin has stretched enough, a permanent implant replaces the expander. Reconstruction with silicone implant will need a flap like latissimus dorsi (LD) flap to cover the silicone prosthesis. This also gives a good result.

Flap Reconstruction:
For those opting for natural tissue reconstruction, tissue is taken from another part of the body, such as the abdomen (TRAM – Transverse Rectus Abdominis Myocutaneous or DIEP- Deep inferior epigastrci perforator flap) are used to create a new breast mound. The surgeon may perform this procedure in one or multiple stages.
Nipple and Areola Reconstruction:
After forming the breast mound, the surgeon creates a nipple and areola to complete the reconstruction. This can involve grafting skin and tattooing to achieve a natural look.
Follow-up and Adjustments:
Post-surgery follow-ups are essential to monitor healing and make any necessary adjustments. Additional procedures may be required to achieve symmetry or improve cosmetic results.
But what about the potential challenges? Here’s what you need to know.
Problems with Breast Reconstruction after Mastectomy
Breast reconstruction after mastectomy, while generally safe, can present several challenges:
- Infection and bleeding are common surgical complications that can delay healing and require additional medical intervention.
- Flap procedures using donor tissue from other parts of the body can lead to complications at the donor site, such as hernias or muscle weakness.

- Implant complications like implant rupture or capsular contracture, where scar tissue causes the implant to feel firm or misshapen, can necessitate further surgeries.
- Scarring in both the reconstructed breast and donor sites (if applicable) can be significant.
- Sensory changes or numbness are common and can be permanent in both the reconstructed breast and donor areas

- Asymmetry between the reconstructed and natural breasts might require additional corrective surgeries.
Are you experiencing complications from breast reconstruction? It is advisable to discuss your concerns with a certified breast reconstruction specialist to explore your options and optimize your recovery.
Wondering what the road to recovery looks like? Let’s walk through it.
Recovery from Breast Reconstruction Surgery after Mastectomy
Recovering from breast reconstruction surgery is a gradual process. It varies based on individual factors, the type of reconstruction performed (implants vs. autologous tissue), and personal healing rates. Always follow the specific guidance given by your surgical team. Here’s a general timeline to help guide expectations:
Immediate Post-Surgery (0-2 weeks)
- Pain and Discomfort: It’s normal to experience pain, swelling, and bruising. Your doctor will prescribe pain medication to manage discomfort.
- Care of Incisions: Drains might be placed to remove excess fluids, and you’ll need to care for your incisions according to your surgeon’s instructions.
- Limited Activity: Avoid strenuous activities and heavy lifting. Most patients are advised to take it easy and focus on recovery.
Early recovery (3-6 weeks)
- Reducing Swelling: Swelling should gradually decrease during this period. Continue to wear any prescribed support garments.
- Increasing Activity: You can slowly start to resume some light activities, as recommended by your healthcare provider.
- Monitoring Healing: Regular follow-up appointments to check your progress and ensure that incisions are healing properly.
Intermediate Recovery (7-12 weeks)
- Improved Mobility: You should start to feel more comfortable moving around and can engage in moderate activities.
- Continued Healing: The appearance of scars will start to improve, although they will still be noticeable.
- Further Follow-ups: These appointments are essential to address any concerns and monitor for complications.
Long-Term recovery (3-6 months and beyond)
- Full Activities: Most patients can return to their regular activities, including exercise, by this stage.
- Final Results Visible: The final shape and appearance of the breast reconstruction will become more apparent.
- Emotional Adjustment: Emotional recovery is also an important aspect, as patients adapt to the changes in their bodies.
Dr. Sandeep Nayak, a surgical oncologist in Bangalore trusted for advanced techniques like robotic breast surgery, advises:
“Ongoing care after breast reconstruction is important, have annual check-ups with your surgeon or oncologist to ensure there are no long-term issues. It is also crucial to monitor the reconstructed breast for any changes or discomfort and report these to your doctor promptly.”
Conclusion
Breast cancer and mastectomy are profound experiences that impact both body and mind. The absence of a breast serves as a constant reminder of the cancer and can make many women feel incomplete or less feminine. Breast reconstruction offers not only a physical transformation but also a significant psychological boost. This procedure not only rebuilds the breast but also restores confidence and a sense of wholeness.
Are you navigating life after a mastectomy? Taking the first step towards recovery and transformation can begin with a consultation. Reach out to a compassionate and experienced surgeon to explore your options for breast reconstruction.
It’s time to start reclaiming your life and achieving the best possible outcomes.
Unveil FAQs about breast cancer after menopause. Let’s get your questions answered.
FAQ
What should I bring to my initial consultation for breast reconstruction?
It’s helpful to bring any relevant medical records, a list of questions you have about the procedure, and a summary of your medical history. This information will assist your surgeon in making informed recommendations tailored to your specific needs.
Can I choose not to have breast reconstruction after a mastectomy?
Yes, opting for breast reconstruction is entirely a personal choice. Some women choose to use prosthetics or not to reconstruct at all, depending on their personal preferences and medical advice.
What is breast prosthesis?
Breast prosthesis is an artificial breast form that can be worn inside a bra to simulate the natural contour of a breast. It is commonly used by women who have undergone mastectomies or other breast surgery to help achieve a balanced silhouette without undergoing reconstruction surgery.
How do I decide between implant-based reconstruction and autologous tissue reconstruction?
The decision typically depends on your body type, medical history, lifestyle, and personal preferences. A consultation with your surgeon will help determine the best approach based on these factors.
Will breast reconstruction interfere with the detection of breast cancer recurrence?
Breast reconstruction should not hinder the monitoring for recurrence. Regular medical exams and imaging tests adapted for your new anatomy can effectively monitor your health.
How long after a mastectomy can I wait to have reconstruction?
You can undergo breast reconstruction during a mastectomy or delay it for months or even years. The timing can depend on your personal circumstances, including your emotional readiness and any additional cancer treatments. If patient does not opt for reconstruction during mastectomy, we prefer to delay the reconstruction at least by 1 year after treatment.


