10 Harmful Effects of Cigarette Smoking on the Respiratory System
Cigarette smoking is one of the leading causes of preventable illness worldwide. While many people know it damages the body, fewer understand just how deeply it harms the lungs. Every puff carries chemicals that slowly weaken breathing capacity, leaving the lungs struggling to function.

According to Dr. Sandeep Nayak, an experienced surgical oncologist in India, smoking not only causes cancer but also a range of chronic respiratory problems that reduce quality of life. Let’s look at the harmful effects in detail.
10 Harmful Effects of Cigarette Smoking on the Respiratory System

Smoking irritates the lining of the airways. Over time, this irritation leads to swelling, excess mucus production, and persistent coughing. This condition is known as chronic bronchitis. Many smokers live with a “smoker’s cough” without realizing it signals long-term damage.

2. Emphysema and Airway Damage
The tiny air sacs (alveoli) in the lungs, which are responsible for oxygen exchange, help you breathe easily. Smoking destroys these delicate sacs, making it hard for oxygen to pass into the blood. This condition, called emphysema, causes breathlessness even during simple activities like walking.

Increased Risk of Lung Cancer
Cigarette smoke contains cancer-causing chemicals. These toxins damage lung cells, increasing the risk of lung cancer significantly. Dr. Sandeep Nayak emphasizes that smoking remains the number one cause of lung cancer worldwide. Early diagnosis and quitting smoking improve survival chances.

Increased Risk of Lung Cancer
Cigarette smoke contains cancer-causing chemicals. These toxins damage lung cells, increasing the risk of lung cancer significantly. Dr. Sandeep Nayak emphasizes that smoking remains the number one cause of lung cancer worldwide. Early diagnosis and quitting smoking improve survival chances.

4. Reduced Lung Function and Capacity
Smokers often notice they can’t keep up with physical activity. That’s because smoking reduces lung capacity. The lungs become less efficient at absorbing oxygen, making even light exercise feel exhausting.

5. Asthma Worsening
For people with asthma, cigarette smoke is a significant trigger. It causes airway tightening, more frequent attacks, and severe breathing problems. Even secondhand smoke can worsen asthma symptoms.

6. Weakened Immune Defense in Lungs
The lungs have natural defenses to fight bacteria and viruses. Smoking weakens these defenses, making it easier for infections such as pneumonia or the flu to take hold. Smokers often take longer to recover from respiratory infections.

7. Chronic Obstructive Pulmonary Disease (COPD)
COPD is a serious combination of chronic bronchitis and emphysema. It develops slowly but leads to permanent breathing difficulties. Many patients realize they have COPD only when it’s advanced, and by then, lung damage cannot be reversed.

8. Increased Risk of Tuberculosis (TB)
Smoking makes the lungs more vulnerable to tuberculosis bacteria. It also weakens the immune response, which means smokers with TB have worse outcomes compared to non-smokers.
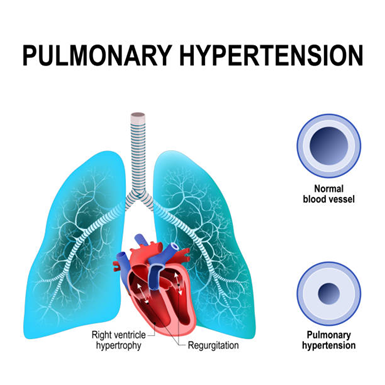
9. Pulmonary Hypertension
Cigarette smoking raises blood pressure in the lungs’ arteries, a condition known as pulmonary hypertension. This makes the heart work harder and can lead to serious complications, including heart failure.

10. Faster Aging of the Lungs
Just like skin, lungs age too. Smoking speeds up this process, making the lungs weaker much earlier in life. Smokers in their 30s or 40s may already experience lung capacity similar to that of non-smokers decades older.
Additional Risks to Non-Smokers

Secondhand smoke is the combination of smoke from a burning cigarette and the smoke exhaled by the smoker. It carries thousands of harmful chemicals, many of which are toxic and cancer-causing. Even brief exposure can irritate the airways, while long-term exposure increases the risk of lung cancer, COPD, and heart disease in non-smokers.
Children face the highest risk. Exposure to secondhand smoke can trigger asthma attacks, frequent coughs, and lung infections like pneumonia. It also slows down lung growth, making breathing more difficult as they grow older.
Prevention and Recovery

The most effective step is to stop smoking. Within weeks of quitting, the lungs begin to repair themselves. Breathing becomes easier, oxygen levels improve, and persistent coughing starts to fade.
Dr. Sandeep Nayak states, “Many harmful effects of smoking can be slowed or even partially reversed with early lifestyle changes and medical guidance.”
Support groups, nicotine replacement therapies, and counseling provide the right support system for those who want to break free from cigarettes.